Fifty year time lapse of the Kidney Failure Program: JAMA
Fifty years ago, then-President, Richard Nixon signed the Social Security Amendments of 1972, which set into motion, the End-Stage Renal Disease (ESRD) program. This program was initiated to provide medical care to patients with chronic kidney diseases.
Technological advances in kidney failure treatment fueled by a political movement, increased the role of the US government in providing kidney failure treatment.
The 1950s, was a time when kidney transplant of discovered as a treatment option for chronic kidney diseases. Dialysis machines and treatment chronic uremia through dialysis was discovered in the 1960s. However, even after the first dialysis centre was established, the treatment of dialysis was still not affordable for the general public
As new dialysis and transplant therapies emerged, enactment of the Medicare entitlement program in 1965 generated momentum toward building a national health system. In this context, the need to ration limited dialysis resources conflicted with commonly held moral sentiments. A 1962 LIFE magazine feature titled “They Decide Who Lives, Who Dies” helped to frame the dilemma through the vivid depiction of a “God committee” tasked with rationing limited dialysis care. The controversial selection processes included consideration of demographics, geography, past and projected occupational performance, and an assessment of moral character. Every congressional body between 1965 and 1972 introduced a bill to expand the government’s role in the financing of treatments for catastrophic kidney disease.1
In 1966, the White House convened an expert committee to review government obligations in the treatment of kidney failure.
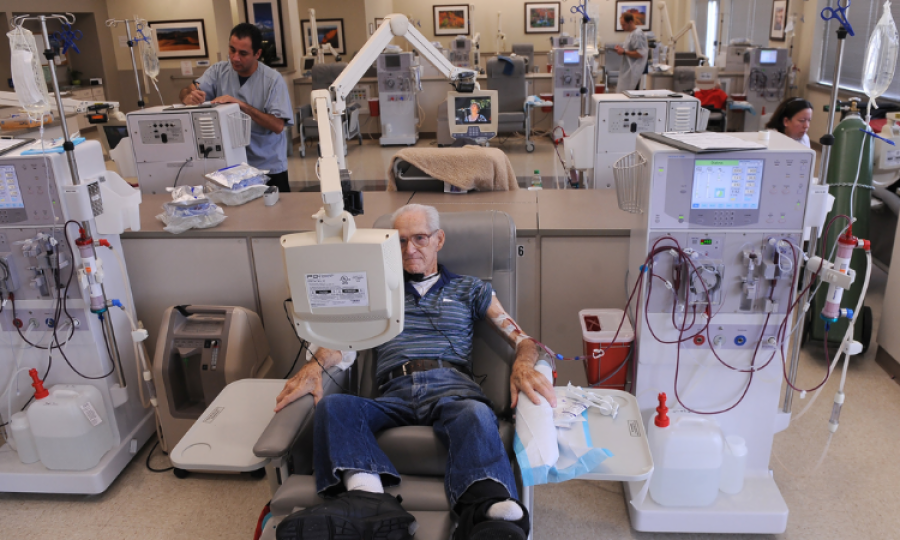
For individuals with kidney failure, the ESRD program was a miracle. By 1980, there were 58 000 patients receiving lifesaving treatment through the program, with enrollment growth averaging 22% per year.
Expansion of patients spanned across all ranges of age, sex, and race, reflecting benefits across broad segments of the US population. Presently, more than 700 000 patients with kidney failure have Medicare coverage.
The US ESRD program has entered a time of transition, in which new challenges coincide with the transition to value-based payment, with uncertain consequences. One major challenge has to do with the structure of the dialysis industry. Dialysis markets have become highly concentrated and remain dominated by for-profit organisations.
Both characteristics may be associated with reduced quality of care and could either help or impede value-based payment reforms. A second challenge involves a changing payer mix. Beginning in 2021, patients with kidney failure became eligible to enroll in Medicare Advantage plans.
Recently, the introduction of a new injectable drug for the treatment of mineral and bone disease led to an increase in the dialysis base payment. If additional technologies have similar effects, growth in per-treatment dialysis costs could reignite, potentially offsetting benefits from the new technologies.
In summary, during its first 50 years the US ESRD program has provided critical access to lifesaving care for many patients with kidney failure. Challenges in balancing cost and quality still persist as the program enters the second half-century of its existence.
Advertisement
Trending
Popular
Hair loss: Discovery uncovers key stem cells that could reverse ...
-
Broccoli sprout compound may help lower ...
11:31 AM, 25 Feb, 2025 -
Gas Pain vs. Heart Attack: How to tell ...
09:00 PM, 22 Feb, 2025 -
Coconut oil supplement shows promise ...
08:00 PM, 20 Feb, 2025 -
Normal vitamin B12 levels may still ...
05:00 PM, 19 Feb, 2025



