Inequity in Paxlovid prescription: JAMA
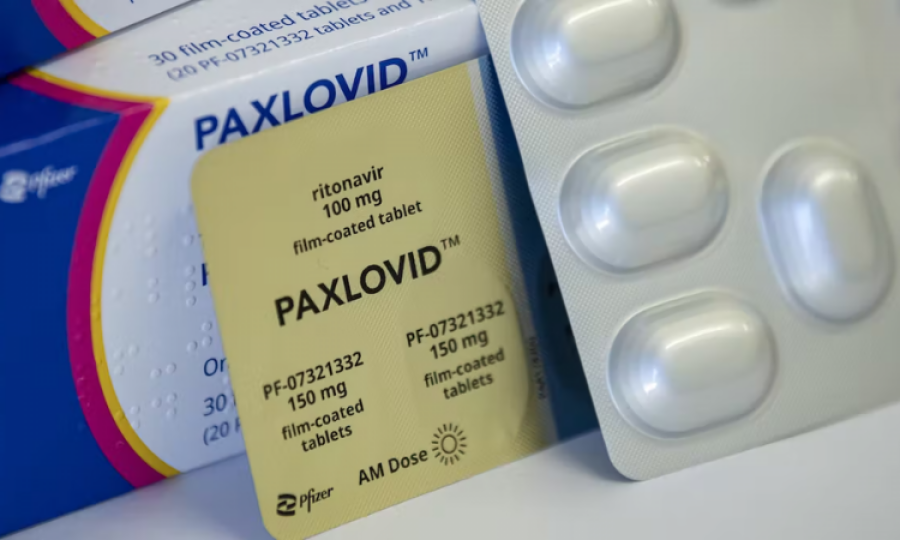
USA: Patients from certain racial and ethnic groups who sought outpatient care for COVID-19 were about 20% to 36% less likely to be prescribed Paxlovid (nirmatrelvir-ritonavir), a multi-institution study found.
The study analyzed the electronic health record data of about 700 000 patients who sought COVID-19 care at 30 sites participating in the National Patient-Centered Clinical Research Network. It found a dramatic increase of patients treated with nirmatrelvir-ritonavir during the study period, from 0.6% in January 2022 to 20.2% in April and 34% in July.
But there were substantial disparities in prescribing. Black patients were 35.8% less likely to be prescribed nirmatrelvir-ritonavir than White patients, and Hispanic patients were 29.9% less likely to be prescribed the drug than non-Hispanic patients.
Nirmatrelvir-ritonavir prescribing was also 24.9% lower for patients who identified as multiple races or “other”; 23.1% lower among American Indian or Alaska Native and Native Hawaiian or Other Pacific Islander patients; and 19.4% lower among Asian patients.
Racial and ethnic disparities also existed in groups at high risk of severe COVID-19. For example, Black patients between the ages of 65 and 79 were 44% less likely to be prescribed nirmatrelvir-ritonavir than White patients in this age cohort. Black, Hispanic, and multiracial or other race patients who were immunocompromised were also less likely to be treated with nirmatrelvir-ritonavir or monoclonal antibodies than non-Hispanic or White patients.
The authors wrote that reduced access to COVID-19 treatment facilities in high-poverty areas or in predominantly American Indian or Alaska Native, Black, or Hispanic communities may have contributed to these disparities.
“Expansion of programs focused on equitable COVID-19 treatment, including raising patient awareness using trusted sources, educating clinicians and other prescribers, and expanding patient access to prescribers, can facilitate equitable health outcomes,” the authors wrote.
Advertisement
Trending
Popular
Aging: New study identifies key lifestyle, environmental factors ...
-
Hair loss: Discovery uncovers key stem ...
08:00 PM, 25 Feb, 2025 -
Broccoli sprout compound may help lower ...
11:31 AM, 25 Feb, 2025 -
Gas Pain vs. Heart Attack: How to tell ...
09:00 PM, 22 Feb, 2025 -
Coconut oil supplement shows promise ...
08:00 PM, 20 Feb, 2025



