What is Crohn’s disease?
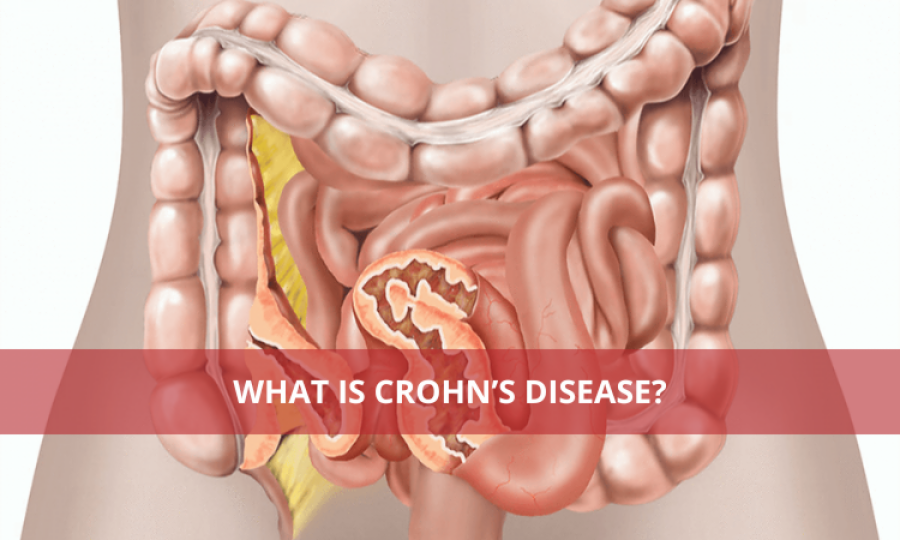
Crohn’s disease is an inflammatory condition of the digestive system. It is a lifelong condition for the patient. It’s a type of inflammatory bowel disease (IBD). It causes the tissues of the digestive tract to swell up and cause a range of symptoms like abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition. The most commonly affected site is the small intestine, but any part of the digestive tract can be affected by it. This disease can be painful and debilitating and occasionally may lead to life-threatening complications. There is no cure for the complete eradication of this disease, but with several therapies, it can lead to the reduction of signs and symptoms, and the normal function of daily life can be resumed. It typically appears in younger people – often in their late teens, 20s or early 30s. However, this condition can happen at any age. It’s equally common in men and women.
Causes
There is no definite cause of this disease, but certain risk factors can increase the chances of getting Crohn’s disease. They include autoimmune disorders, genes and smoking. Often IBD runs in the family; if there is any parent or sibling with this condition, you are more likely to get it too. Apart from this, smoking can mess up the digestive system and put you at risk of Crohn’s disease.
Symptoms
A range of symptoms are experienced by people facing Crohn’s disease. It can be flare-ups or little to no signs. There is no timeline and no predictable pattern as to when the symptoms will arise. Some of the usual and most common symptoms of Crohn’s disease are:
- Abdominal pain
- Chronic diarrhea.
- Fullness or bloating.
- Fever.
- Suppressed appetite.
- Weight loss.
- Abnormal skin tags.
- Anal fissures.
- Anal fistulas.
- Rectal bleeding.
Diagnosis
It is diagnosed by routine examination with complaints of chronic symptoms such as ongoing diarrhea, belly cramping or unexplained weight loss. Doctors then order tests such as blood tests, stool tests, colonoscopies, Computed tomography (CT) scans, and Upper gastrointestinal (GI) endoscopies coupled with an Upper gastrointestinal (GI) exam.
Treatment
Treatment depends upon the severity and the range of symptoms. In children, the goal of therapy is to induce remission (the time between symptom flare-ups), maintain remission and manage any complications of Crohn’s disease over time. Treatment methods may include antibiotic supplements to prevent abscesses and fistulas, antidiarrheal medication like loperamide, monoclonal antibodies to suppress the immune response, Corticosteroids like cortisone and prednisone, bowel rest and even surgery to treat the complications.
Complications
Serious complications of Crohn’s disease include fistulas, bowel obstruction, anal fissures, colon cancer, malnutrition, ulcers, and abscesses. These complications can only be prevented and, if they occur, can be treated with the help of surgery. The management of Crohn’s disease is dependent upon the reduction of complications and decreasing the symptoms. It is a lifelong condition which requires the patient’s compliance, diet modifications and other preventive measures to help battle this incurable disease.
Advertisement
Trending
Popular
Gas Pain vs. Heart Attack: How to tell the difference and when to ...
-
Coconut oil supplement shows promise ...
08:00 PM, 20 Feb, 2025 -
Normal vitamin B12 levels may still ...
05:00 PM, 19 Feb, 2025 -
Revolutionizing Genomic research: The ...
02:00 PM, 19 Feb, 2025 -
Plastic burning for cooking and heating ...
06:15 PM, 18 Feb, 2025



