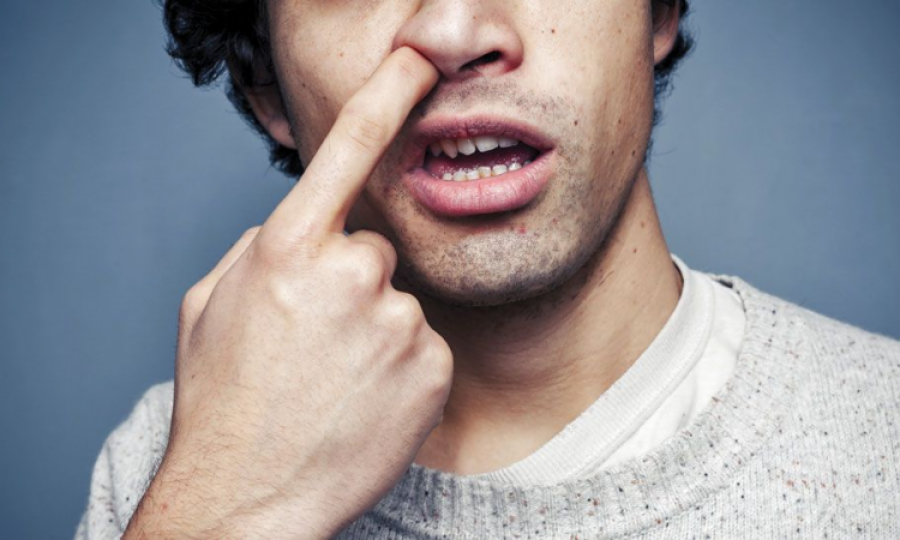
Research claims nose picking can lead to Alzheimers and Dementia
Australia: Griffith University researchers have revealed that bacterial microorganisms can travel through the olfactory nerve system in the nose, to the brain. This research, as demonstrated in mice, has proven that the bacteria can produce markers specific to Alzheimer’s disease.
This study has been published in the journal of Scientific Reports, and shows that Chlamydia pneumoniae used the nasal cavity as a shortcut to the brain, to incade the central nervous system. The cells in the brain then responded by depositing amyloid beta protein which is a hallmark of Alzheimer’s disease.
Co author Prof James St John
Professor James St John, Head of the Clem Jones Centre for Neurobiology and Stem Cell Research, is a co-author of the world first research.
“We’re the first to show that Chlamydia pneumoniae can go directly up the nose and into the brain where it can set off pathologies that look like Alzheimer’s disease,” Professor St John said. “We saw this happen in a mouse model, and the evidence is potentially scary for humans as well.”
The olfactory nerve in the nose is directly exposed to air and offers a short pathway to the brain, one which bypasses the blood-brain barrier. It’s a route that viruses and bacteria have sniffed out as the simplest one into the brain.
The team is currently planning to prove the same pathway exists in humans, in the next phase of their research.
“We need to do this study in humans and confirm whether the same pathway operates in the same way. It’s research that has been proposed by many people, but not yet completed. What we do know is that these same bacteria are present in humans, but we haven’t worked out how they get there.”
Simple steps to look after the lining of your nose have been advised by Professor St John to lower their risk of potentially developing late-onset Alzheimer’s disease.
“Picking your nose and plucking the hairs from your nose are not aadvised”,” he said.
“Bacterial invasion and damage to the inside of your nose is a consequence of nose picking and hair plucking.
“If you damage the lining of the nose, you can increase how many bacteria can go up into your brain.”
Smell tests also have potential as detectors for Alzheimer’s and dementia says Professor St John, as loss of sense of smell is an early indicator of Alzheimer’s disease. He suggests smell tests from when a person turns 60 years old could be beneficial as an early detector.
“Once you get over 65 years old, your risk factor goes right up, but we’re looking at other causes as well, because it’s not just age—it is environmental exposure as well. And we think that bacteria and viruses are critical.”
This research was supported by the Goda Foundation and the Menzies Health Institute Queensland.
Advertisement
Trending
Popular
Aging: New study identifies key lifestyle, environmental factors ...
-
Hair loss: Discovery uncovers key stem ...
08:00 PM, 25 Feb, 2025 -
Broccoli sprout compound may help lower ...
11:31 AM, 25 Feb, 2025 -
Gas Pain vs. Heart Attack: How to tell ...
09:00 PM, 22 Feb, 2025 -
Coconut oil supplement shows promise ...
08:00 PM, 20 Feb, 2025



